NEUROENDOCRINE CANCER OF THE
APPENDIX
The Facts
Neuroendocrine Neoplasm (NENs) is an umbrella term used to cover a group of cancers that start in neuroendocrine cells. These cancers may also be referred to as NETs, NECs, or even Carcinoids. NENs occur when neuroendocrine cells stop working normally and start to grow or behave abnormally.
There are 2 key types of NEN:
- NETs (neuroendocrine tumours) are called ‘well-differentiated’ and tend to have a slow to moderate growth pattern.
- NECs (neuroendocrine carcinomas) – are called ‘poorly differentiated’ and tend to grow rapidly.
To simplify, we use the term NENs throughout this page.
Appendix NENs
The appendix can be found near the junction where the large and small bowel meet. It is a small thin tube, approximately 4 inches long. Normally the appendix sits in the lower right abdomen. It has no clearly identified function in humans.
Appendix NENs are uncommon, however, they do make up the majority of Appendicial Neoplasms. They are usually only discovered following treatment, for example, histology review following appendicectomy. Symptoms, if they occur, tend to be the same as for suspected appendicitis. Most of the tumours are located at the tip of the Appendix and are diagnosed at an early stage, meaning that curative surgery can be performed. A small proportion are located at the base of the Appendix and may require further and longer term interventions.
Symptoms
Symptoms that may or may not include Neuroendocrine Cancer associated syndromes. (Syndrome is where 2 or more related symptoms occur).
Neuroendocrine Cancers of the appendix are uncommon and usually only discovered during tests or treatments for other conditions, for example, histology review following appendicectomy. Therefore symptoms, if they occur, may be the same as for suspected appendicitis.
They are rarely associated with a Neuroendocrine Cancer associated syndrome.
Tests
Tests that may be used for the diagnosis and / or monitoring of Neuroendocrine Cancer of the Appendix:
Blood and / or urine:
Full blood count
Liver and kidney function
CEA, Ca19-9, Ca-125.
Chromogranin A
Urinary or serum 5HiAA (serotonin).
Scans:
CT chest & abdomen and / or CT chest &MRI abdomen
Octreotide (SPECT) or Gallium-Dotatate PET/CT.
Endoscopy:
Colonoscopy or CT colonoscopy/enterolysis (a non-invasive CT examination of the large/small bowel)
Pathology (what can be seen through special tests under a microscope):
Differentiation and cellular morphology
Synaptophysin
Chromogranin
CEA.
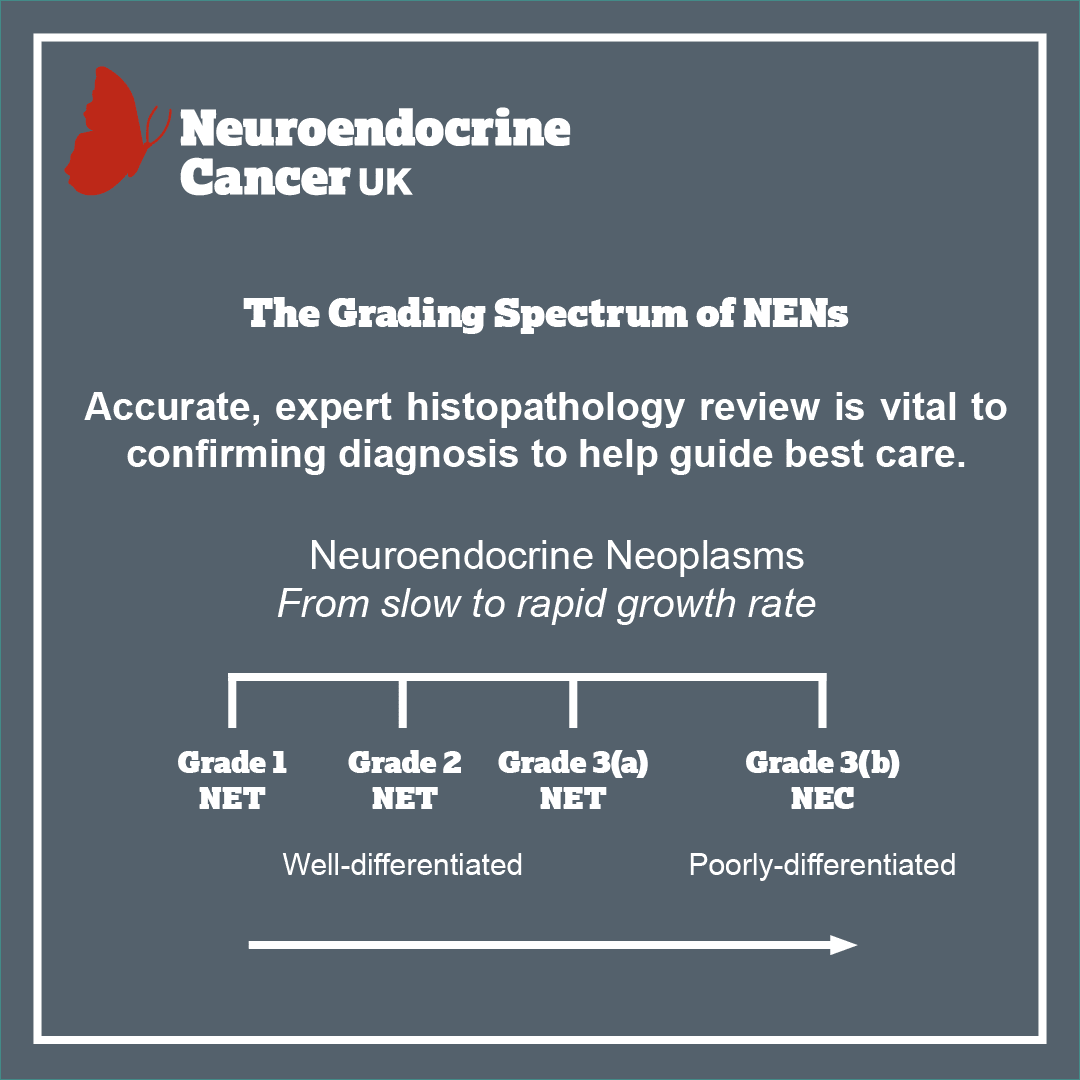
Grading
Not all cancers are the same or behave in the same way. Some may grow very slowly, may not have invaded nearby structures, or spread to other parts of the body at the time of diagnosis – but they have the potential to. However some may have already spread at the time of diagnosis. The grade is the rate at which the NEN grows. You might see this referred to as ‘Ki67’ or ‘Mitotic Index’ mentioned in your clinic letters or medical reports. Grade 1 is slow-growing through to Grade 3, a more aggressive, rapidly growing disease.
So how is it treated?
For all patients, there are many things to consider in planning treatments. Your treatment will be personalised to you and the type of NEN you have. Even if you have a diagnosis that sounds the same as another patient, your treatment and follow up plan may be different.
The key aim of treatment, should be to help you have the best possible care and quality of life, by ensuring access to appropriate treatment, management of symptoms and addressing what’s most important to you.
One or more of the approaches below may be suggested:
- Removal of all or part of your NEN
- Control of your disease, by slowing or stopping the growth of your NEN
- Palliation, or easing of your symptoms.
Treatment options include:
- Surgery
- Surveillance – can be used to assess how well treatment is working or in periods between treatments (which may be months/years).

Appendiceal NENs, less than 1cm, completely removed by surgery, often do not need any further treatment or follow up – they are essentially cured. However, if the NEN is larger, shows evidence of spread, is found at the base of the appendix or the appendix has ‘burst’, you may need further follow up and/or treatment.
Your care team will discuss your treatment options with you – giving you both written and verbal information – to help you make an informed choice. Together you can agree on the most appropriate treatment for you.
There is consensus agreement that all NEN patients should be reviewed by a specialist MDT.
Treatment options will depend on the type, position and size of your NEN, and whether (or to where) it has spread. It will also depend on whether you have any other health concerns and / or illnesses and your general health and fitness. A big part of meeting with your doctors or specialist nurse/team, is to make sure you get the information you need to understand your condition.

Follow up
There are expert agreed guidelines regarding how and when follow up should occur, however, in practice this varies and often with good reason. Follow up should be expert informed & evidence /research based but also tailored to you and what is appropriate for your best care.
Following appendicectomy:
Less than 1cm, completely resected (R0):
- Well-differentiated neuroendocrine tumour (WDNET), Grade 1 (Ki67 <2%), lymph node negative with no evidence of further disease
- NO follow up required beyond routine post-op check.
More than 1cm, less than 2cm, completely resected (R0):
- WDNET, Grade 1, NO evidence of mesoappendiceal or angio-invasion or further disease
- A single post-op CT chest/abdomen – if clear, NO further follow up required
If there is any evidence of further disease (e.g. enlarged locoregional lymph nodes), a right hemicolectomy and lymph node assessment is recommended.
If further surgery is not undertaken or other risk factors* are present then longer-term follow up is recommended.
Risk factors* include tumour found at base of appendix, mesoappendiceal invasion > 3mm, grade 2 (Ki67 3-20%) or evidence of vascular invasion.
More than 2cm:
- Grade 1 or 2, with or without angioinvasion or deep mesoappendiceal infiltration and / or lymph node involvement
- CT chest/abdo/pelvis 6-12 monthly with annual Chromogranin A for a minimum 7 – 8 years.
Following right hemicolectomy:
- If no evidence of residual disease – no lymph nodes or metastases: NO further follow up is required
- Where there is evidence of lymph node and / or distant metastases – follow up as per >2cm
- Biochemistry (CEA, Ca19-9, Ca 125 +/- Chromogranin A) may be used a surrogate markers
- Colorectal surveillance as per national Improving Outcome Guidance (IOG) protocols.
Advanced disease:
Follow up as per guidelines – but should be guided by prognosis, expected treatment efficacy and treatment related toxicity. Your health, well-being, physical activity, informed choice and preference for ongoing care as well as aim of treatment should be reviewed and discussed to best plan care.

