Hi I’m Martin, 57 years old, long-term Pancreatic Neuroendocrine patient. 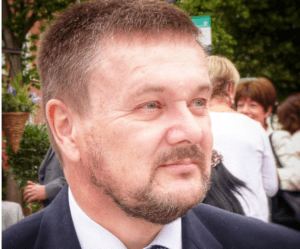
I guess all good stories need to have a good beginning. I can probably trace the start of my relationship with Neuroendocrine Cancer back to 26 January 2003. Why so accurate? It was Super Bowl weekend, I was in Orlando working on a project for a Turkish Bank, I watched the game in a restaurant eating supersized American food, all washed down with copious jugs of beer. The next day I had a stomach pain which was bad enough to keep me off work for a day.
On returning to the UK, I had a health check through work, which suggested I could be pregnant! Following referral for further investigation, I had an operation to remove a gallstone and the gallbladder. During the operation the surgeon identified pancreatic lesions, although I was not informed that they were neuroendocrine tumours. I was referred to a Gastroenterologist who implemented a program of scans to monitor the pancreas.
Late 2009 the scans confirmed tumour growth in the pancreas.
Early 2010, an endoscopic biopsy confirmed I had Pancreatic Neuroendocrine Tumours. It was stressed that this was not (aggressive) Pancreatic Cancer and that NETS were generally slow growing and not cancer. Even so, I was referred for surgery and advised that the tumours could be removed from the pancreas (like plucking golf balls off blancmange) with a worst-case scenario that they might also have to remove the head of the pancreas. The night before the operation I was advised, by a junior doctor, that the surgeon had changed his mind and planned to undertake a Total Pancreatectomy. This unexpected, last-minute change meant that both myself and the ward staff were totally unprepared for the challenges of diabetes and insulin dependency. My first post-operation memory was having Ketoacidosis and readmission to ITU, the ward hadn’t realised I needed my blood sugar closely monitored and insulin prescribed to control my blood sugar.
Following the operation understanding, managing and living with diabetes took priority.
I continued with the now familiar program of scans (now under the Oncology department) until 2014, when an 11-hour operation saw the surgeon undertake the removal of more lymph nodes, the resection of retroperitoneal lesions, and the repair of an incisional hernia (a result of the previous operations).
Again, I had no treatment to manage future disease progression, however the regular scans continued with no evidence of recurrence and in 2017 it was agreed that after the next annual scan in 2018 the monitoring would be scaled back to every two years as it was thought that the risk from ongoing scans was greater than that from NETs.
Based on this positive prognosis, I agreed to take redundancy and we seized the opportunity to relocate from London to semi-rural Cheshire.
(Just a quick side-track from the health stuff, throughout this period I continued to work on large software projects. How was the quality of my work? I was still receiving top grade feedback and assessments. However, in retrospect, the time taken to achieve the same quality and quantity of work did noticeably increase over time to the detriment of family life…)
Having returned to London for the 2018 scan, we were advised at the follow up consultation that I now had multiple liver metastases. I suppose we should not have been surprised that for the second time these slow growing, non-aggressive tumours had suddenly become an issue.
To cut down on future travel for monitoring and treatment I was referred to Professor Valle at The Christie, Manchester. After 14 years, it was time to see a Neuroendocrine specialist and team!!!
Following the diagnosis of Inoperable Liver Metastases, I am now receiving my first treatment (other than surgery) for Neuroendocrine Cancer, prescribed Lanreotide Injections every 28 days.
I’m not sure if it’s the reduced functionality of the liver, the impact of the Lanreotide, or both, but there has been a significant impact on the balance / workings of my body, which I had previously been able to maintain with Insulin and Creon.
It was whilst at the initial consultation, at The Christie, that we were invited to a Neuroendocrine Cancer Conference in Manchester. It was the first time Neuroendocrine Cancer had been fully explained to us. I met Neuroendocrine specialists, listened to many mind-blowing presentations, and met fellow Neuroendocrine patients for the first time. It was a revelation.
Since that conference, Neuroendocrine Cancer UK has played a significant role in me being able to accept my new norm. The Natters are always informative (thanks Nikie) and just listening to the experiences of fellow Netters seems to help, even when they are talking about conditions and symptoms I cannot relate to.
Following the diagnosis in 2018, I became active on various Facebook Groups (Neuroendocrine, UK Whipple, Pancreatic Cancer, Total Pancreatectomy) learning from the experiences of others and trying to share my experiences where appropriate.
Joining the Neuroendocrine Patient Ambassador Team means that I will have a more concrete platform to share my historic and future experiences (watch out for future Blogs / Vlogs) whilst utilising the consultancy skills built up over 30 years, to assist with the various reviews and projects planned for the team. I also understand that the Team will be looking to offer additional support, in the near future, in addition to the current Natter program. Hopefully when launched these new services will also be well used. Personally, as I am no longer working, I’ve been missing a sense of purpose and becoming a Patient Ambassador brings with it an opportunity to make a difference and to add some value.
Hopefully, before too long, the Patient Ambassadors will be able to get out and about providing support at conferences and charity events. I hope to make it to the Great North Run this year to support my daughter who will be running in aid of Neuroendocrine Cancer UK. So, if you are in the North East come on down, have a chat, and put some money in the Neuroendocrine buckets.
To close, a quick summary of life today… My daughters who were 7 and 4 at the start of this journey have somehow remained perfect – beautiful, intelligent, supportive, and well balanced. Nicky my wife, and rock, has managed to stay the course – although I do think she enjoys giving the Lanreotide injections a little too much. We have escaped the rat race and found a quiet life in a small village. Two years age we expanded our family to include a gorgeous Sprocker Spaniel and I would recommend a dog to anyone. Maya is great therapy, providing a reason for exercise and always aware when you are down or not feeling quite right. The diabetes remains a 24*7 challenge. I’ve progressed to an insulin pump integrated with a continuous glucose monitor. Its an amazing piece of kit…. for a Type 1 diabetic, I’m waiting for the next development, a dual pump incorporating glucagon as well as insulin to fully replicate what I’m missing from my Pancreas and Liver function. I intend to hang around long enough to take advantage of this advancement.
