NEUROENDOCRINE CANCER OF THE
LARGE BOWEL
The Facts
Neuroendocrine Neoplasm (NENs) is an umbrella term used to cover a group of cancers that start in neuroendocrine cells. These cancers may also be referred to as NETs, NECs, or even Carcinoids. NENs occur when neuroendocrine cells stop working normally and start to grow or behave abnormally.
There are 2 key types of NEN:
- NETs (neuroendocrine tumours) are called ‘well-differentiated’ and tend to have a slow to moderate growth pattern.
- NECs (neuroendocrine carcinomas) – are called ‘poorly differentiated’ and tend to grow rapidly.
To simplify, we use the term NENs throughout this page.
Large Bowel NENs
The large bowel is also known as the large intestine or colon. It forms the last part of the digestive system leading to the rectum. As food passes through the digestive system it is broken down and the nutrients we need to survive are extracted. By the time it reaches the colon it is mostly fluid and waste product. Bacteria in the colon breaks down any remaining substances and water is absorbed – whatever remains passes into the rectum to be excreted as waste (‘stool’).
Bloating, gas and pain may be experienced if the colon isn’t working properly; diarrhoea and, or constipation can occur. Irritation of the lining of the colon or damage such as a tumour forming can lead to bleeding which may appear in the stools, as blood, or the stool may be black and tarry.
NENs of the Large Bowel can be NETs or NECs. Sometimes NENs can occur in combination with the more common Large Bowel (Colon) Cancer, either as completely separate cancers within the large bowel or as one cancer containing both kinds of cancer cell, this is called MiNEN (mixed Neuroendocrine nonNeuroendocrine Neoplasm).
Symptoms
Symptoms that may or may not include Neuroendocrine Cancer associated syndromes. (Syndrome is where 2 or more related symptoms occur).
Symptoms of Neuroendocrine Cancer of the Colon may be very similar to those that occur in Bowel Cancer, and include:
- A persistent change in your bowel habits, including diarrhoea or constipation or a change in the consistency of your stool
- Rectal bleeding or blood in your stool (may make it look black / tar-like)
- Persistent abdominal discomfort, such as bloating, cramps, gas or pain
- A feeling that your bowel doesn’t empty completely
- Weakness or fatigue
- Unexplained weight loss
However, many people experience no symptoms in the early stages of the disease. When symptoms appear, they may be related to the cancer’s size and location.
They are not usually associated with a Neuroendocrine associated syndrome – those that may produce Carcinoid Syndrome are more commonly found in the ascending colon (the first part of the large bowel) or where Neuroendocrine Cancer may have spread to the liver.
Other, rarer symptoms, including Paraneoplastic syndrome and oncological emergencies, (a specific set of health concerns that can occur in any cancer), such as raised calcium levels (Hypercalcaemia), may occur.
Further information about Neuroendocrine Cancer associated and Paraneoplastic Syndromes – including Oncological emergencies – can be found here.
Tests
Tests that may be used for the diagnosis and / or monitoring of Neuroendocrine Cancer of the Large Bowel:
Blood and / or urine:
Full blood count
Liver and kidney function
B12/Iron/Ferritin/Folate
Chromogranin A
Urinary or serum 5HiAA (serotonin).
CEA
Beta-HCG
Scans:
CT chest, abdomen and pelvis and/ or CT chest & MRI abdomen and pelvis
Octreotide (SPECT) or Gallium-Dotatate PET/CT
FDG-PET
Endoscopy:
Colonoscopy +/- biopsy
Pathology (what can be seen through special tests under a microscope):
Differentiation and cellular morphology
Synaptophysin
Chromogranin
Ki67
Low molecular weight keratins
GLP
PP/PYY
CD56.
Select play to watch a short video where Professor Martyn Caplin talks to us about Large Bowel Neuroendocine Neoplasms.
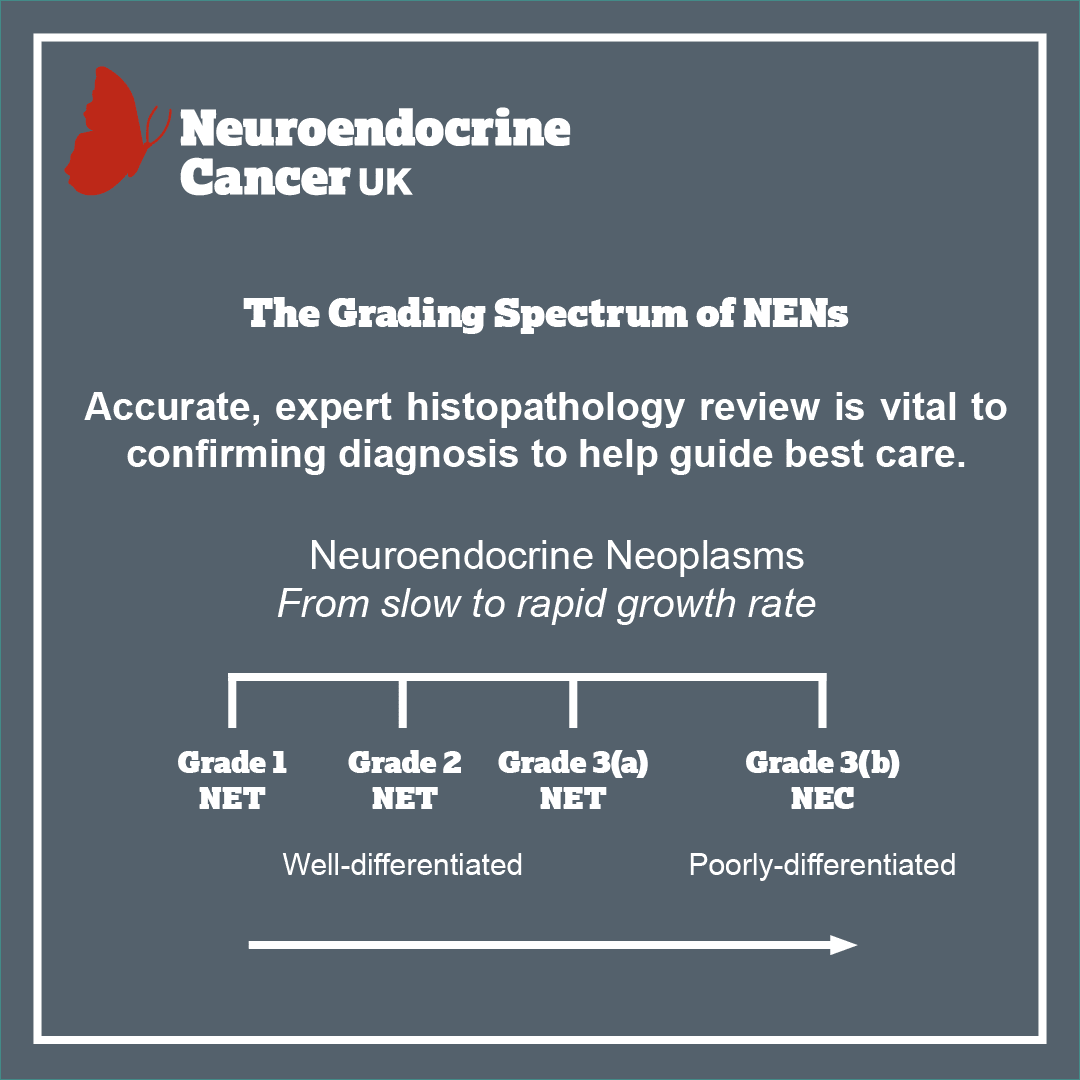
Grading
Not all cancers are the same or behave in the same way. Some may grow very slowly, may not have invaded nearby structures, or spread to other parts of the body at the time of diagnosis – but they have the potential to. However some may have already spread at the time of diagnosis. The grade is the rate at which the NEN grows. You might see this referred to as ‘Ki67’ or ‘Mitotic Index’ mentioned in your clinic letters or medical reports. Grade 1 is slow-growing through to Grade 3, a more aggressive, rapidly growing disease.
Select play to watch a ‘Spotlight on Small and Large Bowel Neuroendocrine Cancers’ video by Dr Raj Srirajaskanthan.
Select play to watch Dr Raj Srirajaskanthan discuss small and large bowel Neuroendocrine Cancers. This video was recorded as part of the Neuroendocrine Cancer UK Virtual Summit 2020.
Causes and / or risk factors
We do not know exactly what causes NENs, however research is ongoing, to truly understand both the pathology and the biology with the hope that this will lead to a much better understanding of the causes. Most NENs do not run in families; however, there are a number of rare conditions that may increase your risk. Therefore, if other members of the family have been diagnosed with a particular cancer (especially aged 50 years or less) or cancer-associated genetic condition, it is important that you tell your specialist team about not only your medical history, but also any family medical illnesses or conditions.
So how is it treated?
For all patients, there are many things to consider in planning treatments. Your treatment will be personalised to you and the type of NEN you have. Even if you have a diagnosis that sounds the same as another patient, your treatment and follow up plan may be different.
Your care team will discuss your treatment options with you – giving you both written and verbal information – to help you make an informed choice. Together you can agree on the most appropriate treatment for you. There is consensus agreement that all NEN patients should be reviewed by a specialist MDT.
Treatment options will depend on the type, position and size of your NEN, and whether (or to where) it has spread. It will also depend on whether you have any other health concerns and / or illnesses and your general health and fitness. A big part of meeting with your doctors or specialist nurse/ team, is to make sure you get the information you need to understand.

The key aim of treatment, should be to help you have the best possible care and quality of life – by ensuring access to appropriate treatment, management of symptoms and addressing what’s most important to you. Treatment options will depend on the type, position and size of your cancer – and whether (and to where) it has spread. It will also depend on whether you have any other health concerns and / or illnesses and your general health and fitness.
One or more of the approaches below may be suggested:
- Surgery
- Control of your disease, by slowing or stopping further growth and / or spread
- Palliation, or easing, of any symptoms you may be experiencing.
Surveillance:
Monitoring through clinic review, bloods and scans, can be used to assess how well treatment is working or in periods between treatments (which may be months/years).
As not everyone will need to be on treatment – surveillance can be used to check your cancer and general health for any signs of change that may mean that a treatment might need to be considered. All treatments have possible side-effects, therefore, it is important to know when treatment may be helpful for you or not.
Surgery:
May be offered to remove the part of the colon that contains the cancer and the nearby lymph nodes, then where possible rejoins the non-tumour part of the bowel back together (the join is called an anastomosis) Surgery to remove part of the colon is called a colectomy – there are several types of colectomy:
Right hemi-colectomy:
Removes the ascending colon +/- ileo-caecal valve.
Extended R hemi-colectomy:
Removes ascending and transverse colon
L hemi-colectomy:
Removes the descending colon
Hartmans procedure:
Sigmoid colon and top part of the rectum and may require a temporary stoma*
Sub-total colectomy:
Removes all of the colon apart from the rectum and anus
Procto-colectomy:
Removes the whole colon and rectum
Pan-proctocolectomy:
Removes the whole colon, rectum and anus – requiring a permanent stoma*
If the cancer is very small (or contained within a polyp) – local resection may be offered – through either surgery or colonoscopy.
Surgery may also be offered to relieve symptoms of or bypass cancer than can not be removed.
*A stoma is formed by bringing part of your colon (large bowel) or the end or loop of ileum (small bowel) out on to the surface of your abdomen – and may be temporary or permanent depending on how much bowel you have left or how healthy your remaining bowel is. Waste passes out of the stoma and is collected in an external pouch (known as a stoma bag).
A large bowel stoma is called a colostomy and a small bowel stoma is called an ileostomy. Waste from an ileostomy is usually more liquid than from a colostomy as it leaves the body before passing through the colon (where water is often reabsorbed).
Non-surgical Treatments:
- Somatostatin analogues (SSAs)
- Chemotherapy
- Targeted Molecular Therapies
- Peptide receptor radionuclide therapy (PRRT)
- Radiotherapy
- Endoscopic procedure
- Interventional radiology
- Clinical Trials
- Symptom Control.

Follow up
There are expert agreed guidelines regarding how and when follow up should occur, however, in practice this varies and often with good reason. Follow up should be expert informed & evidence /research based but also tailored to you and what is appropriate for your best care.
Following surgery/endoscopic resection – for minimum 10 years:
- G1/2 <1cm: no lymph nodes, no evidence of invasion: there is no data re recommended follow up.
- G3 <1cm: annual follow up with colonoscopy.
- G1/2 1-2cm: annual follow up with colonoscopy.
Biochemistry alongside colonoscopy/scan.
ALL Neuroendocrine Cancers >2cm require ongoing follow up – minimum 10 years (nb metastatic disease has been seen beyond this time):
- G1/2: annual colonoscopy + CT + biochemistry.
- G3: 4 – 6 monthly colonoscopy + CT + biochemistry for the first year, then annually.
If liver tumours present – for MRI or contrast CT concurrent with follow up timings.
Advanced disease:
Follow up as per guidelines – but should be guided by prognosis, expected treatment efficacy and treatment related toxicity. Your health, well-being, physical activity, informed choice and preference for ongoing care as well as aim of treatment should be reviewed and discussed to best plan care.

